Restless Leg Syndrome and Impulse-Control Disorders in Parkinson’s Disease: Observational study
Document Type : Original Communication
Authors
1 Department of Neurology, Sanjay Gandhi Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
2 Department of Microbiology, All India Institute of Medical Sciences, Bilaspur, Himachal Pradesh, India
3 Department of Psychiatric Social Work, National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru, Karnataka, India
Abstract
Background: Impulse-control disorders and related behaviors (ICD-RB) and restless leg syndrome (RLS) are common in Parkinson’s disease (PD) patients, but their relationship and independence from dopaminergic therapy are not well understood. This study aims to determine the correlation between ICD-RBs and RLS and the significant psycho-behavioral profile of RLS patients in the presence of ICD-RBs.
Methods: The study screened PD patients visiting a neurology outpatient department for addictive behaviors, alcohol and substance abuse, and ICDs using the QUIP questionnaire. RLS was diagnosed based on the criteria set by the International RLS study group. The cohort was divided into groups based on the presence of ICDs and RLS.
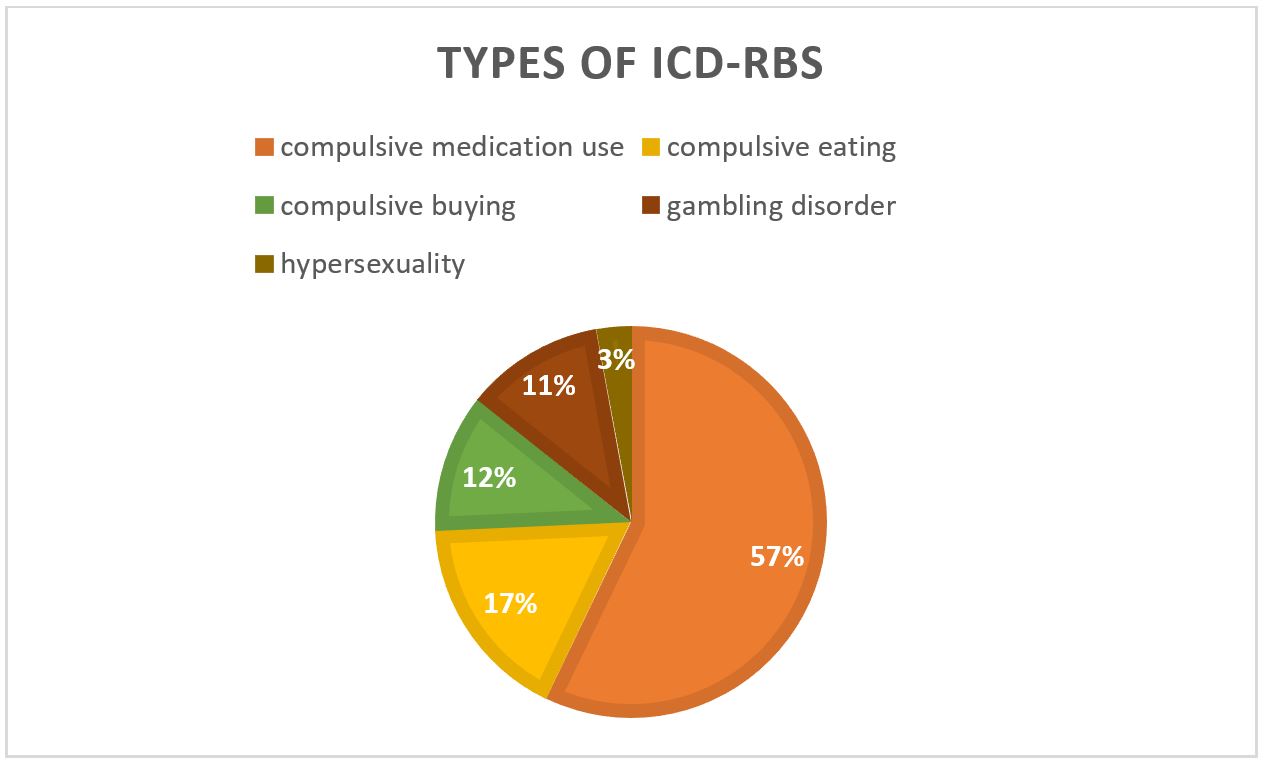
Results: 48.6% of the 72 PD patients in the study displayed at least one Impulse Control Disorder-Related Behavior (ICD-RB), with 57.1% showing compulsive medication use, 17.1% showing compulsive eating, 11.4% showing compulsive buying, 11.4% displaying gambling disorder, and 2.8% displaying hypersexuality. In addition, 26.3% of patients in the cohort had Restless Legs Syndrome (RLS), with 68.4% of these patients displaying at least one ICD-RB. Among patients with RLS and ICD-RBs, gambling was the most commonly observed behavior, displayed by 30.7% of patients, while 36.8% displayed co-occurring compulsive eating. Only one patient showed more than one ICD-RB, which included both gambling and compulsive medication use.
Conclusion: The study concludes that 11% of PD patients can have co-occurrence of RLS and ICD-RBs, and this behavioral profile may be due to circadian fluctuation in dopamine release in a hyper-dopaminergic state. Long-term dopaminergic treatment or degenerative processes may be the cause of both RLS and ICD-RBs in PD patients.
Keywords
Main Subjects
Introduction
Parkinson's disease (PD) is a progressive neurodegenerative disorder that requires the use of dopaminergic medications to manage motor symptoms (1). However, the use of dopaminergic drugs has been associated with the development of Impulse control disorders and related behaviors (ICD-RBs) in some patients, particularly those with a young age of disease onset, male gender, and pre-existing addictive personality traits (2). It is unclear whether PD itself confers an increased risk of ICD-RBs. While literature has not demonstrated an increased risk of ICD-RBs in PD patients in the absence of treatment, some symptoms suggestive of ICD-RBs have been reported in newly diagnosed, untreated PD patients(3).
Restless leg syndrome (RLS) is also common in PD patients, and several studies suggest a shared neuropathology between PD and RLS. The occurrence of RLS is associated with progressive dopamine depletion, which may play a role in its development (4). However, RLS and ICD-RBs represent two sides of the coin in PD patients, as the occurrence of one requires dopamine treatment, while the other is a result of an excess of dopamine. Additionally, studies have reported addictive gambling behavior in untreated idiopathic RLS patients, suggesting that these impulsive behaviors may be related to specific predisposing patient profiles associated with the disease (5, 6).
Therefore, the current study aims to determine any correlation between the co-occurrence of ICD-RBs and RLS in PD patients and to study whether the presence of RLS is associated with any significant psycho-behavioral profile in the presence of ICD-RBs.
Methods
The present research was conducted as a hospital-based observational cross-sectional study at the neurology department of a tertiary care hospital located in India. Written informed consent was obtained from all study participants after explaining the primary purpose of the study. The study aimed to investigate patients clinically diagnosed with idiopathic Parkinson’s disease and on dopaminergic therapy with levodopa and/or dopamine agonist for at least twice daily doses for a minimum of one year, with no changes in their dopaminergic therapy for the last month. Patients responsible for maintaining their daily medication were also included. However, patients with cognitive dysfunction (MMSE <24), on antidepressant therapy, and those with secondary Parkinsonism (multiple system atrophy, progressive supranuclear palsy, vascular PD) were excluded from the study. The demographic data of the patients, including their age, gender, rural/urban residence, and occupation, were collected using a structured questionnaire. Disease characteristics, including complete details of treatment, levodopa (LD), dopamine agonist (DA), as well as the calculation of levodopa equivalent daily dose (LEDD), type of PD, age of onset, duration of the disease, H and Y stage, UPDRS-III score (ON state), and other co-morbidities, were recorded. Any history of addictive behaviors, alcohol, and substance abuse was also recorded. The authors evaluated and recorded ICDs with the help of a QUIP questionnaire, which was translated into vernacular language and used in their previous study.
Impulse Control Disorders (ICDs)
To evaluate the presence of Impulse Control Disorders (ICDs) in patients with Parkinson's disease, the researchers used the Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s Disease (QUIP). Both patients and their informants, such as caregivers or spouses, were instructed to complete the QUIP questionnaire. They were asked to answer the questions based on the behaviors that occurred anytime during the disease for at least four consecutive weeks. The questionnaire assessed the presence of ICDs and was divided into three sections. The first section consisted of five questions, including an introductory question describing problem behaviors, for the four most common ICDs reported in Parkinson's disease. The second section contained three distinct introductory questions and two additional questions for hobbyism, punding, and walkabout. The third section had five questions, including an introductory question, for compulsive medication use. The optimal cut-off point for each ICD was used to determine the presence of ICD-RBs: gambling (affirmative answers to ≥2 questions), sexual behavior (≥1 question), buying (≥1 question), and eating (≥2 questions). Hobbyism, punding, and walkabout were recorded in the questionnaire. Compulsive medication use was noted based on the patient's responses to the questionnaire (item 1 and 4) [9].
As part of an extension attached to the QUIP questionnaire, the authors studied certain presentations of Impulse Control Disorders (ICDs) not covered by the questionnaire, which may be relevant in the Indian population. These included body-focused repetitive behaviors (trichotillomania, hair nibbling, skin picking, nail biting, cheek biting, nose picking), hypergraphia, and pyromania in patients with Parkinson's disease. This was previously studied by the authors [10].
Restless Legs Syndrome
To evaluate Restless Legs Syndrome (RLS), the diagnostic criteria set by the International Restless Legs Syndrome Study Group were used. These criteria consisted of four questions, all of which had to be answered 'yes' for a patient to be diagnosed with RLS. After patients met the criteria, they were evaluated and confirmed by a neurologist.
Statistical analysis
The data obtained from the study were analyzed using IBM SPSS Statistics 26. Descriptive statistics, including means, standard deviations, percentages, and frequencies, were used to analyze demographic and clinical parameters. The range and median of H and Y stages were also calculated. Chi-square tests were used to analyze categorical variables such as gender, rural/urban residence, occupation, education, substance abuse, presence of ICD and corresponding type, compulsive medication use, and any other compulsive behaviors. T-tests were used to analyze quantitative variables such as the age of the patient, duration of the disease, levodopa equivalent daily dose, and daily dose of the dopamine agonist. The level of statistical significance for all tests was set at ≤0.05.
Results
Out of the 107 patients with Parkinson's disease (PD) who visited the OPD during the study period, 72 eligible participants were included in the study. The cohort consisted of 38 (52.7%) males and 34 (47.2%) females, with a mean age of 62.4 (+8.6) years. The mean duration of PD was 4.2 years, and the median H and Y stage was 3. In this cohort, 52 (72.2%) participants were on levodopa, 20 (27.7%) patients were on dopamine agonist treatment, and 33 (34.7%) participants were
receiving both dopaminergic drugs. Out of 72 PD patients, 35 (48.6%) had at least one Impulse Control Disorder-Related Behavior (ICD-RB), while 37 (51.4%) PD patients had no ICD. Additionally, 19 (26.3%) patients had Restless Legs Syndrome (RLS), while 53 (73.6%) did not have RLS.
Among PD patients with ICD-RBs, compulsive medication use was seen in 20 (57.1%) patients, compulsive eating in 6 (17.1%), compulsive buying in 4 (11.4%), gambling disorder in 4 (11.4%), hypersexuality in 1 (2.8%) (Figure 1). The other compulsions noted were hand washing, reading, internet use, listening to music, watching television, stitching, and arranging flowers in pots.
Of the 19 PwPD with RLS, 13 patients (68.4%), were found to have at least one ICD-RBs. Out of these 13 patients, 7 were males (53.8%) and 6 were females (46.1%). Gambling was the most commonly observed compulsive behavior in the PD-RLS group, with 4 patients (30.7%) displaying this behavior (P < 0.0001). Co-occurring compulsive eating was also significantly associated with RLS, with 7 patients (36.8%) displaying this behavior. Only one patient showed more than one ICD-RB, which included both gambling and compulsive medication use.
Discussion
The current investigation aimed to establish the possible connection between restless legs syndrome (RLS) and impulse control disorders (ICDs) in patients with Parkinson's disease (PwPD). The results of the study show that more than half (53.6%) of the participants had at least one ICD-RB, with compulsive drug intake being the most common, while 18.9% of PwPD experienced RLS. Moreover, 12.6% of PD patients had both RLS and at least one ICD-RB. The study also explored the association between RLS and specific ICD-RBs. The results indicated that gambling (27.7%) and compulsive eating (44.4%) were the most common ICD-RBs observed in the presence of RLS, while hypersexuality was reported by only 5.5% of patients.
The study also investigated the development of compulsive medication overuse, specifically Dopamine dysregulation syndrome (DDS), which is characterized by compulsive misuse and addiction to dopamine replacement therapy. DDS is more commonly observed in older individuals, while other RCD behaviors are more prevalent in patients with a younger age at disease onset (7, 8). DDS appears to be linked to a family history and previous drug abuse. Two-thirds of DDS patients may also have other ICDs due to shared risk factors (9). However, in the current study, only one patient with RLS was among 25 patients with compulsive medication overuse.
Thirteen PD patients with RLS showed a higher preference for ICBs compared to PD patients without RLS, possibly due to the temporal association between RLS and these behaviors (10, 11). Patients with compulsive eating reported increased nocturnal eating behavior, while gambling was more prevalent in the evening or at night, which could disrupt sleep and explain the association with RLS (12-14). Conversely, poor sleep quality and increased daytime sleepiness due to RLS were found to increase the likelihood of impulsive behaviors in PD patients (15-17). The study also highlighted the circadian fluctuation of dopamine levels as a possible mechanism for the co-occurrence of RLS and ICBs in PD patients (18). Further research is necessary to confirm this circadian modulation of ICBs. Previous studies have shown that sleep disruption, regardless of the cause, is a risk factor for abnormal behaviors. The presence of a circadian profile of dopamine levels, in addition to dopaminomimetic drugs, may contribute to the coexistence of RLS and nocturnal compulsive behaviors in PD patients (19, 20). Lastly, in later stages of PD, a dopamine deficiency may occur in the nigro-striatal pathway, causing hypersensitivity of D1 and D2 receptors primarily located in the dorsal striatum, and dopaminergic medications may lead to desensitization of dopamine receptors (21).
Conclusion
Given the study's small sample size, the causal relationship between ICBs and RLS can only be inferred as an association or co-existence, and further research is needed to determine whether specific behaviors are risk factors for RLS or vice versa. The study's limitations include potential underestimation of RLS due to treatment and the absence of a control group. Despite these limitations, the study revealed unique findings, such as the co-occurrence of RLS and ICD-RBs in 12.6% of PD patients, and suggested that circadian fluctuations in dopamine levels on a background of hyper-dopaminergic states may explain the emergence of both RLS and ICBs in PD patients. Long-term dopaminergic treatment or the degenerative process itself may contribute to this behavioral profile. Further research is warranted to confirm these findings in larger samples.
Declarations
Funding
We do not have any financial support for this study.
Conflict of interest
The authors have no conflicts of interest to disclose.
Availability of data
The datasets analyzed during the current study are available upon request with no restriction.
Code availability
Not applicable
Consent for publication
This manuscript has been approved for publication by all authors.
| 1. Tolosa E, Wenning G, Poewe W. The diagnosis of Parkinson's disease. Lancet Neurol. 2006;5(1):75-86. https://doi.org/10.1016/S1474-4422(05)70285-4 PMid:16361025 |
||||
| 2. Akdemir Ü, Bora Tokçaer A, Atay L. Dopamine transporter SPECT imaging in Parkinson's disease and parkinsonian disorders. Turk J Med Sci. 2021;51(2):400-10. https://doi.org/10.3906/sag-2008-253 PMid:33237660 PMCid:PMC8203173 |
||||
| 3. de Almeida CMO, Brito MMC, Bosaipo NB, Pimentel AV, Sobreira-Neto MA, Tumas V, et al. The Effect of Cannabidiol for Restless Legs Syndrome/Willis-Ekbom Disease in Parkinson's Disease Patients with REM Sleep Behavior Disorder: A Post Hoc Exploratory Analysis of Phase 2/3 Clinical Trial. Cannabis Cannabinoid Res. 2023;8(2):374-8. https://doi.org/10.1089/can.2021.0158 PMid:35749710 |
||||
| 4. Zhang PL, Chen Y, Zhang CH, Wang YX, Fernandez-Funez P. Genetics of Parkinson's disease and related disorders. J Med Genet. 2018;55(2):73-80. https://doi.org/10.1136/jmedgenet-2017-105047 PMid:29151060 |
||||
| 5. Winkelmann J, Schormair B, Lichtner P, Ripke S, Xiong L, Jalilzadeh S, et al. Genome-wide association study of restless legs syndrome identifies common variants in three genomic regions. Nat Genet. 2007;39(8):1000-6. https://doi.org/10.1038/ng2099 PMid:17637780 |
||||
| 6. Sobreira-Neto MA, Pena-Pereira MA, Sobreira EST, Chagas MHN, Almeida CMO, Fernandes RMF, et al. Is restless legs syndrome in Parkinson disease patients associated with any specific factor? Arq Neuropsiquiatr. 2021;79(1):38-43. https://doi.org/10.1590/0004-282x-anp-2020-0122 PMid:33656110 |
||||
| 7. Wu K, Politis M, Piccini P. Parkinson disease and impulse control disorders: a review of clinical features, pathophysiology and management. Postgrad Med J. 2009;85(1009):590-6. https://doi.org/10.1136/pgmj.2008.075820 PMid:19892894 |
||||
| 8. Clemens S, Rye D, Hochman S. Restless legs syndrome: revisiting the dopamine hypothesis from the spinal cord perspective. Neurology. 2006;67(1):125-30. https://doi.org/10.1212/01.wnl.0000223316.53428.c9 PMid:16832090 |
||||
| 9. Hayes MT. Parkinson's Disease and Parkinsonism. Am J Med. 2019;132(7):802-7. https://doi.org/10.1016/j.amjmed.2019.03.001 PMid:30890425 |
||||
| 10. Jankovic J. Parkinson's disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry. 2008;79(4):368-76. https://doi.org/10.1136/jnnp.2007.131045 PMid:18344392 |
||||
| 11. Jahan I, Hauser RA, Sullivan KL, Miller A, Zesiewicz TA. Sleep disorders in Parkinson's disease. Neuropsychiatr Dis Treat. 2009;5:535-40. https://doi.org/10.2147/NDT.S4578 PMid:19898667 PMCid:PMC2773284 |
||||
| 12. Tippmann-Peikert M, Park JG, Boeve BF, Shepard JW, Silber MH. Pathologic gambling in patients with restless legs syndrome treated with dopaminergic agonists. Neurology. 2007;68(4):301-3. https://doi.org/10.1212/01.wnl.0000252368.25106.b6 PMid:17242339 |
||||
| 13. Iranzo A, Comella CL, Santamaria J, Oertel W. Restless legs syndrome in Parkinson's disease and other neurodegenerative diseases of the central nervous system. Mov Disord. 2007;22 Suppl 18:S424-30. https://doi.org/10.1002/mds.21600 PMid:17534950 |
||||
| 14. Minar M, Kosutzka Z, Danterova K, Gmitterova K, Straka I, Kusnirova A, et al. Restless legs syndrome in Parkinson's disease: relationship with quality of life and medication. Bratisl Lek Listy. 2022;123(1):55-60. https://doi.org/10.4149/BLL_2022_009 PMid:34967659 |
||||
| 15. Lv Q, Wang X, Asakawa T, Wang XP. Pharmacologic Treatment of Restless Legs Syndrome. Curr Neuropharmacol. 2021;19(3):372-82. https://doi.org/10.2174/1570159X19666201230150127 PMid:33380302 PMCid:PMC8033969 |
||||
| 16. Stefani A, Högl B. Sleep in Parkinson's disease. Neuropsychopharmacology. 2020;45(1):121-8. https://doi.org/10.1038/s41386-019-0448-y PMid:31234200 PMCid:PMC6879568 |
||||
| 17. Winkelmann J, Allen RP, Högl B, Inoue Y, Oertel W, Salminen AV, et al. Treatment of restless legs syndrome: Evidence-based review and implications for clinical practice (Revised 2017)(§). Mov Disord. 2018;33(7):1077-91. https://doi.org/10.1002/mds.27260 PMid:29756335 |
||||
| 18. Högl B, Stefani A. Restless legs syndrome and periodic leg movements in patients with movement disorders: Specific considerations. Mov Disord. 2017;32(5):669-81. https://doi.org/10.1002/mds.26929 PMid:28186669 |
||||
| 19. Trenkwalder C, Allen R, Högl B, Paulus W, Winkelmann J. Restless legs syndrome associated with major diseases: A systematic review and new concept. Neurology. 2016;86(14):1336-43. https://doi.org/10.1212/WNL.0000000000002542 PMid:26944272 PMCid:PMC4826337 |
||||
| 20. Silva MME, Lorenzi CH, Schneider BB, Seidel CEF, Salomé I, Gianini VCM, et al. Restless legs syndrome in Parkinson's disease and increased cardiovascular risk. Arq Neuropsiquiatr. 2018;76(11):731-5. https://doi.org/10.1590/0004-282x20180114 PMid:30570015 |
||||
| 21. Rijsman RM, Schoolderman LF, Rundervoort RS, Louter M. Restless legs syndrome in Parkinson's disease. Parkinsonism Relat Disord. 2014;20 Suppl 1:S5-9. https://doi.org/10.1016/S1353-8020(13)70004-X PMid:24262188 |
||||
Volume 2, Issue 1
April 2023Pages 51-54
- Receive Date: 09 May 2023
- Accept Date: 02 June 2023
 Neurology Letters
Neurology Letters
